Foal

Failure of Passive Transfer
Foals are born without a fully developed immune system and they rely on the transfer of antibodies from the first milk (colostrum) directly into the blood stream as whole proteins called Immunoglobulins. This mechanism, called Passive Transfer, only occurs for the first 6-12 hours of life after which the gut “closes” to complete antibodies. Therefore from birth to 12 hours of age the foal must ingest adequate, good-quality colostrum, to have good immunity; if insufficient colostrum or if that colostrum is too poor quality, the foal will have a poor immune system with the likelihood of infection, septicaemia and potentially death.

Immunoglobulin G (IgG) levels are an indication of the effectiveness of passive transfer and normally should be above 8g/L to provide good immunity. Partial immunity or partial passive transfer (PPT which is between 4-8g/L) provides some protection but that may be overwhelmed by infection. Less than 4g/L is regarded as failure of passive transfer (FPT) and provides poor, inadequate immunity and there is a high risk of infection leading to septicaemia and death.
Routine blood sampling of the foal should be done from 24-36 hours of age to evaluate the IgG levels. Depending on the result there is the option to administer hyper-immune plasma from donor horses which has high levels of IgG (usually >24g/L) to provide the antibodies (and immune system) to the foal.
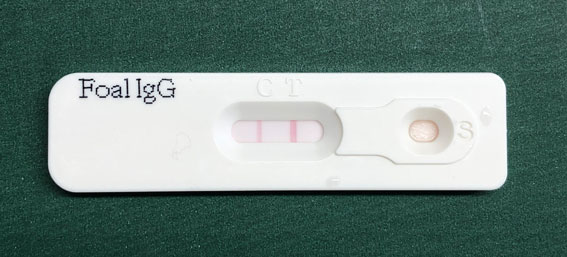
There are several foal-side tests but a very common one is an ELISA test:-
If the level is <4g/L then hyper-immune plasma is essential.
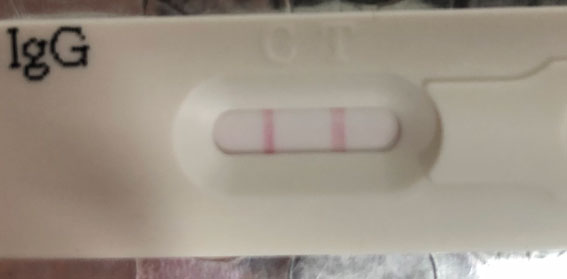
If the level is 4-8g/L then hyper-immune plasma is recommended.
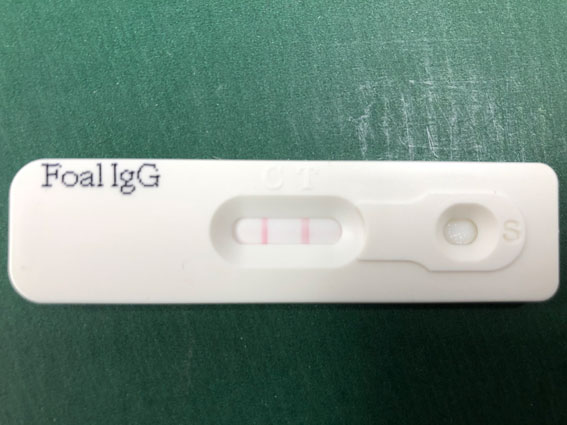
If the level is >8g/L then hyper-immune plasma is unnecessary.
Administering the plasma to the foal needs to be done once the FPT or PPT is identified to reduce the risk of infection taking hold. Commercially available plasma can be frozen for up to 2 years and contains a minimum of 24g/L of IgG. The antibodies have a cross-reaction against Escherichia coli (E. coli) and Salmonella species and are commonly used in treatment of any endotoxaemia (adult or foal). In most cases the frozen plasma is defrosted carefully over a few hours using warm water not more than 40oC. Defrosting MUST NOT be done in the microwave or using hot water which can damage the antibodies by destroying the proteins. The plasma is then administered via an intravenous cannula using a blood-giving set which has a special filter to ensure fibrin clots are removed. Commonly the foal is sedated with diazepam or α2 sedatives, although this may not be necessary if the foal is weak or already collapsed.
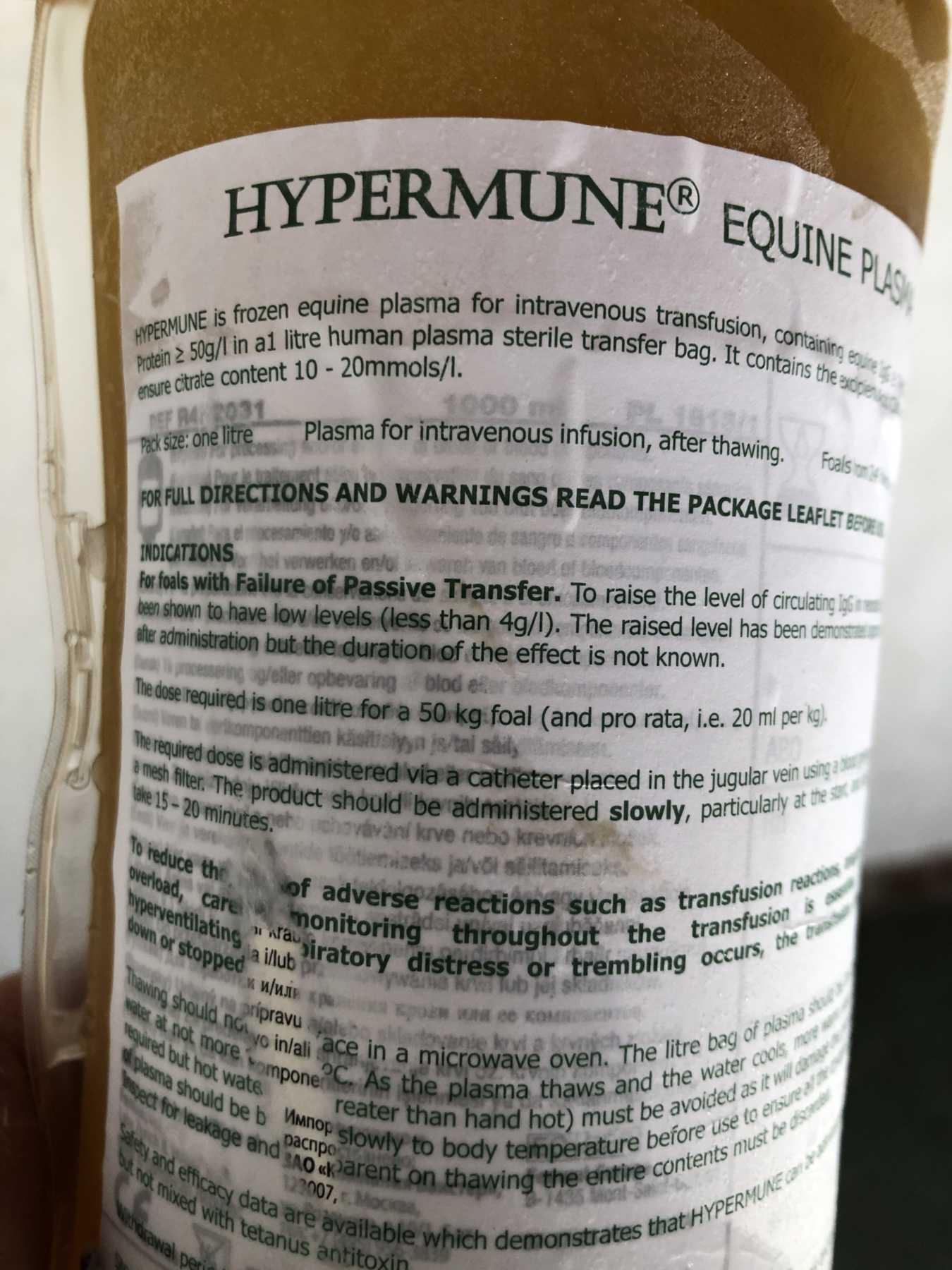
Normally one litre of plasma is given over a period of 15-30 minutes whilst closely monitoring the foal’s heart and respiratory rates; if anything abnormal is noticed then the rate of administration is slowed.
A blood sample may be taken 24 hours later to recheck the IgG levels and ensure that they have increased above 8g/L. If not, the plasma may be repeated 24-36 hours after the first litre.
This does not give a guarantee against any infection but it does give a good fighting chance.
An alternative to the “normal” equine plasma is a commercially available plasma containing antibodies against Rhodococcus (Corynebacterium) equi. This can be a devastating disease in some stud farms with widespread illness in foals up to 6 months of age. The main sign is a bronchopneumonia although lesions may occur in the intestines.
On stud farms where R. equi is endemic, RE plasma can be given at birth and again at 25-45 to attempt protection against this dreadful disease at the most critical times.
Providing plasma by intravenous infusion has certain risks such as reactions to the “foreign” protein material in the plasma and in severe cases, anaphylaxis. Careful monitoring is always carried out and the speed of administration may be reduced if heart or respiratory rates increase. Steroids or adrenaline may be given if severe reactions are observed.
On the whole it is very safe and a life-saving treatment for many foals who would, without it, have died as a result of sepsis.